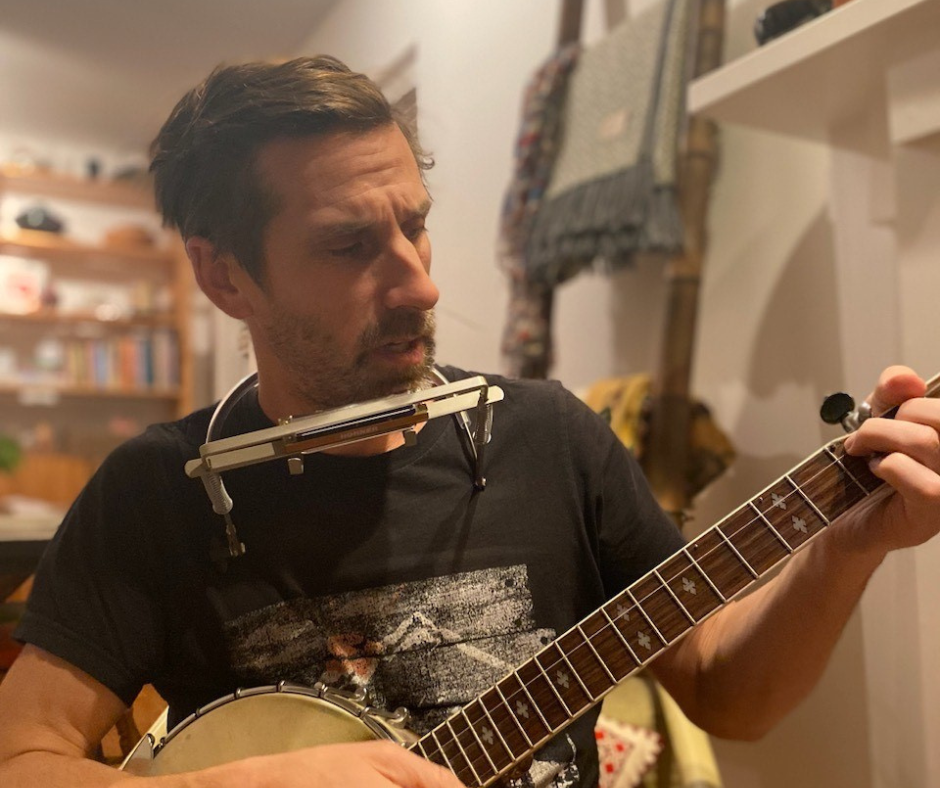
Michael Politano-Bowles:
Spiritual Health Practitioner, Victoria General Hospital; writer, musician, friend, uncle, son, human
Spiritual Health Practitioners are here for patients, families, and hospital staff. It’s unique because we’re one of the only roles in the hospital that takes care of the staff too.
The trick is, what is spiritual? Sometimes spiritual can be religious. For example, if someone is experiencing a stressful situation, they might want prayer. Faith is an important part of their life. If we can support them religiously and in a way that is authentic to us as practitioners, that’s great. If not, we’ll liaise with the community to find someone who can meet those religious needs.
But when we talk about spiritual needs, we’re really talking about meeting the needs of the human spirit.
When someone is in the hospital, something in their life has changed. They’re distressed, they’re disconnected from their sense of meaning, or they’ve lost touch with their sense of purpose. They might feel isolated. Whether they have family or not, it’s really about helping them find groundedness through their relationships and their sense of meaning, and helping them connect to internal resources that they might already have, but are easy to forget in distressful situations. Really, my role is largely about reminding people of their innate ability to be resilient.
I think the biggest comfort to people is being heard. When patients can talk to somebody who’s non-judgmental, and compassionate, and for them to be able to share their stories and a part of themselves while being heard and understood and respected, I think that brings the most comfort. Hospitals are busy places and they can be isolating. Spiritual Health Practitioners have the privilege and honour of being able to give people quality time and connection to explore who they are as people and what they value.
Generally, I feel like I’m always trying to get people back into their story. And if they’re inviting me into their story, it’s also reminding them of who they are and what’s important to them—because that’s what is so easily forgotten.
“Really, my role is largely about reminding people of their innate ability to be resilient.”
“What I end up providing is a little closer to what we would call psychological first aid. It’s really just allowing people to decompress with whatever they’re carrying.”
I think story is what makes us so uniquely human. So much of despair is actually lack of connection to story—or when we’ve lost touch with our own story. It’s what gives us a sense of connection and that deep sense of belonging that we all have a hunger for. We all have a story that connects us to others who have one. Our stories resonate with each other. It’s just about allowing them to live and allowing them to come out of us.
Sometimes, if a patient has a loved one or friend who can bring something familiar from home, it can act as a sort of touchstone or grounding presence. It’s a way to bring us out of the story that all chaos is breaking loose and refocus the narrative that gives someone strength, purpose, and meaning.
To me, my role is about being present, and I truly believe that’s what people want. Curiosity is the best word we have to describe the work of spiritual health. If you have a tradition or a set of values and beliefs and you want to tell me about it, that empowers you to educate me. That might change the dynamic of the relationship and allow you to feel safe and trust me, which can help to shift perspectives, give new meaning, and transform someone’s hospital experience. Curiosity means I don’t need to know a lot about any particular religion, faith, or tradition to be genuine and authentic, and to fulfill my role as a Spiritual Health Practitioner.
When I’m working with hospital staff, particularly in this context and this time, what I end up providing is a little closer to what we would call psychological first aid. It’s really just allowing people to decompress with whatever they’re carrying—whether that’s something in their personal life that is affecting their work life, or something that has directly come out of an experience in the work environment. It’s really just creating and holding space for staff to be able to come and let their guard down, and share a little of what they’re feeling so they can decompress and reset.
Over the course of doing this work for the last seven years, I don’t find myself getting hardened or emotionally burdened, but I think my own practices are definitely a part of that. I do physical practices like yoga, music and singing, which are ways to just move the energy through. When I talk to people about grief, I tell them the energy has to move through us—if it stays there, that’s when the problems start. I also have my own contemplative practice. I really benefit from doing practices that are physical, embodied, and that help me let go of things I might otherwise hold on to.
Outside of the hospital, I walk and hike a lot. I read. I love to write, and I’ve reconnected with storytelling quite recently. It’s sort of a lost art that I dropped and I’m now putting energy back into—which feeds my work as well because so much of it is about story.
On an ideal day off, I might spend the morning with my cat Beatrice and then go get a coffee and do some reading. Then I’d meet up with a friend for lunch and do some writing in the afternoon, before getting out in the garden if only to watch the birds. For dinner, I’d go to my parents’ place for my mom’s lasagna and hang out with my nephew. My family is mostly Victoria-based, and my sister has only recently been here, so I’ve been reconnecting with her and my nephew over the last year. After all of that, I’d come home and play music with friends. That would be the ultimate day.
My hope for people for the holidays is to find a place where there’s warmth. There are lots of people out there looking for connection and togetherness regardless of where they’re at, and my encouragement would be for people to take whatever risk they need to take to open their heart to others. That’s the hard thing. It’s hard to be vulnerable in moments when you feel things like despair and isolation. But when we start to think of things like connection and story as medicine, that’s when we’re truly starting to value their role in healing and transforming people’s lives.
“There are lots of people out there looking for connection and togetherness regardless of where they’re at, and my encouragement would be for people to take whatever risk they need to take to open their heart to others.”
They are humans first, who put other humans first.
More than 8,900 caregivers and staff work around the clock in our Victoria Hospitals
#HumansFirst is dedicated to sharing the stories from behind our hospitals’ frontlines. These stories remind us that those who provide care and keep the lights on in our hospitals also have lives outside of them. They have family and friends, they enjoy hobbies and interests, and they have all lived through their own personal triumphs and heartbreaks. Like all of us, they are human, and they have a story to tell.