Research project: Reducing spasticity by harnessing the power of nitrous oxide
Spasticity is a disabling condition that affects hundreds of thousands of Canadians living with neurological disorders, including stroke, cerebral palsy, multiple sclerosis, and brain injuries. Spasticity robs people of the use of their limbs, and can be deforming and painful. This team has developed a treatment to deep-freeze nerves with nitrous oxide gas using a tiny probe through the skin. The result is muscle relaxation, restored function for shoulders, arms, hands, and hips, knees, feet, and improved quality of life for many patients. ($88,000)
VHF: Can you tell us about your research project?
Dr. Winston: We treat a condition called spasticity. It is a neurologic disorder that, for the purposes of this project, can happen after a stroke. Pain in the shoulder is the fourth most common disability after stroke, and the most common cause of pain. It’s so disabling that some people can’t participate in rehab. Many of these patients are paralyzed or have a high resistance to movement, which is what we call spasticity. People can’t use the limb that is affected by spasticity.
Our project aims to treat these people within the first weeks to months after their stroke so that we can eliminate their pain as much as possible, and stop their spasticity from getting worse. Otherwise, people get permanently deformed limbs that they can’t move. We’re trying to alter the course of that progression and offer immediate treatment so that they can participate in rehab and stop taking their medications—including opioids.
The second part is treating the pain in hips and knees from arthritis that prevents patients from getting out of bed or transferring to their chair, walking or participating in exercise. We freeze the nerves that carry pain to the hip and knee.
VHF: What do you think is the most innovative part of your project?
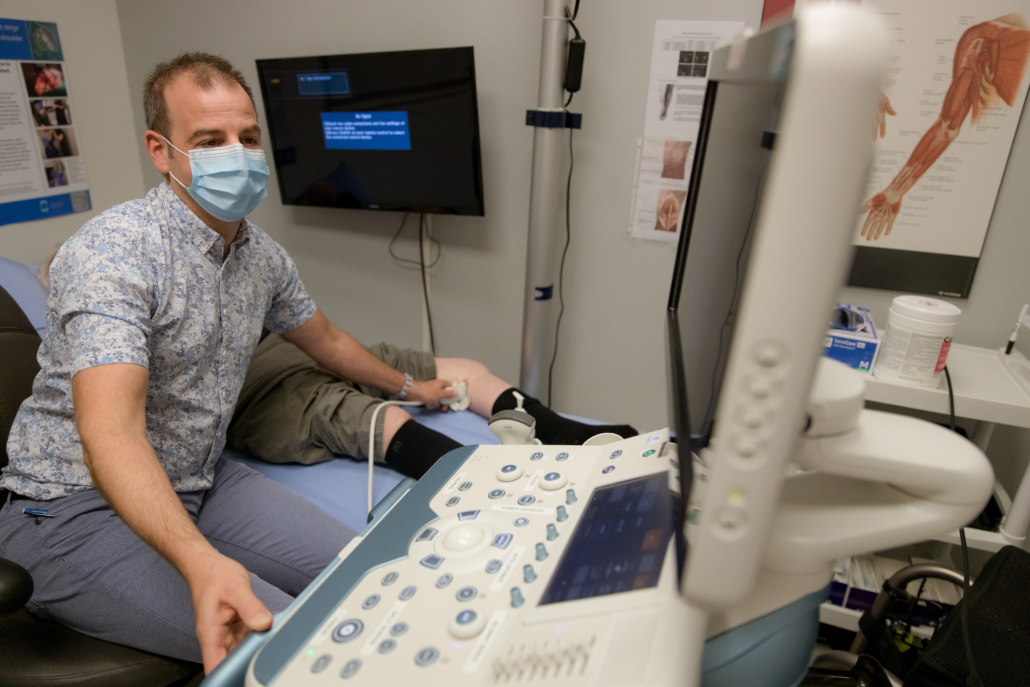
Dr. Winston: This novel use of the technology was designed in Victoria, and now it’s spreading around the world quickly. We’re presenting it everywhere, and I really do think it’s going to become a global practice. And the innovation is that we can go right to the patient’s bedside to offer this treatment, thanks to the portable ultrasound that donors funded through the Victoria Hospitals Foundation. We do the procedure and it has an instant effect. The patient can suddenly start moving their limb, or they tell us they no longer have pain.
We’ve had cases where there’s a patient upstairs who needs an overhead lift just to get up and down, and after this treatment, all of a sudden all the nurses are clapping because this 90-year-old patient is walking. Or there might be a patient who can’t use their arm, and they’re crying and they’re on opioids. They have their treatment and the next time we see them, we ask them how they are. And they can say they’re fine.
VHF: How does this project improve someone’s quality of life?
Dr. Winston: Pain from stroke can basically condemn some patients to never functioning in society again. It might be too painful for someone to walk, or they might not be able to even dress or feed themselves. After treatment, we see many of these patients transform. Even if they don’t gain more movement, the pain goes away. They’re sleeping through the night. They’re not taking opioids or painkillers. It’s been really exciting for us to see that. For some people, the results are dramatic.
We’ll often treat an inpatient at the end of the day. Each patient is different, but the excitement is the look on a therapist’s face when they come back in the morning and they say, “What did you do to my patient? They’re a new person!”
VHF: Donors currently have an opportunity to help fund a $44,000 physiatry ultrasound. Can you explain how this equipment enables in your work?
Dr. Winston: We cannot do this procedure without the ultrasound, which helps us locate the correct nerves to freeze.
We have also just published the world’s first atlas on how to do ultrasound procedures for spasticity, and having really beautiful, high-tech ultrasound images was a big part of what made that possible.
VHF: What is the most meaningful part of this project for you?
Dr. Winston: What’s so meaningful for me is that it’s a really human project. It’s taking suffering and something that robs people of their independence and mobility, and giving them back as much as possible. We’re giving people back their freedom, their autonomy, and it has been very rewarding.
VHF: How does support from our giving community fuel your work?
Dr. Winston: Support from the community means we can create projects that meet the needs of our community. The community supports us by funding equipment through the Foundation. Ongoing supports means we can continue to build on projects they have already supported. We can keep building until we get even better.
To be supported by the people of Vancouver Island, and to be able to give back to the Island, is just amazing. Support from the community allows us total freedom to do this work.
VHF: What does the word innovation mean to you?
Dr. Winston: To me, innovation means the freedom to rebuild. We look at our skillsets and patients and ask questions like, “What if there’s a better way that is cheaper, more effective, and safer? What if we can get rid of the use of medications?” Right now, I’m saving about $6,000 per year for each patient I treat just in drug costs alone.
VHF: What gives you hope for the future?
Dr. Winston: One of the things that gives me hope is a project that I call “Project Hand.” It’s about restoring really good hand function to people so that they can hold their spouse’s hand and walk together or touch their parent’s face. It’s a very emotional experience for people. We cry a lot in our clinic. Magic happens here.



